Your vital lung capacity: Why is it important and how can you improve it with yoga?
The last time I visited my mom, she asked me to show her some yoga moves because she wasn’t feeling too well. Once we got down to the floor, I asked her to take a few full, deep breaths. She could barely inhale for two seconds and exhale for two seconds. This immediately sent alarm bells through my brain since I’d never seen anybody breathe in such a shallow way. It felt very, very wrong. My mom passed away three months later. This was ten years ago.
The connection between vital lung capacity and mortality has been known for some time now. It was first described scientifically by researchers in the Framingham Heart Study, which has been going on since 1948 and is now considered one of the longest, most important epidemiological studies in medical history. The researchers have made many discoveries over the years regarding risk factors for cardiovascular diseases. In 1983, they published a research paper based on 20 years of biannual follow-up of 5209 subjects that placed vital lung capacity at the top of those risk factors. Vital lung capacity is usually determined by measuring the amount of air that can be forcibly exhaled from your lungs after taking the deepest breath possible. This is called FVC (forced vital capacity).
The researchers wrote: “FVC was strikingly related to the incidence of cardiac failure at all ages and in both sexes. The association persisted even after adjustment for age, cigarette smoking, and hypertension, as well as for other cardiovascular risk factors [height, weight, heart rate, and glucose intolerance]. The strong relationship to the development of cardiac failure indicates that the simple vital capacity is a sensitive indicator of impaired cardiac function. […] Vital capacity appeared to rank high as a predictor among the major risk factors for cardiovascular morbidity as well as for mortality.”(1)
The researchers were not exactly sure why it was happening but had some interesting ideas: “The explanation for the remarkable association between FVC and cardiovascular morbidity and mortality is at present rather speculative. … There is one intriguing correlation which may provide a clue; the strongest correlation observed for FVC is with handgrip strength. This suggests that the FVC may well be a measure of overall vigor and general strength.”(1) Could it be that our vital lung capacity is indeed an indicator of our overall vitality?
Multiple studies have been conducted since then (see resources below for some examples), and most of them came to similar conclusions. By now, it is widely accepted that vital capacity is a reliable predictor of one’s mortality. Forced vital capacity test puts a number to your vital capacity – it shows how much air you can take into your lungs and then actively expel. The ability of your lungs to do that depends on two key factors: lung compliance and lung elasticity. Let’s look at those more closely.
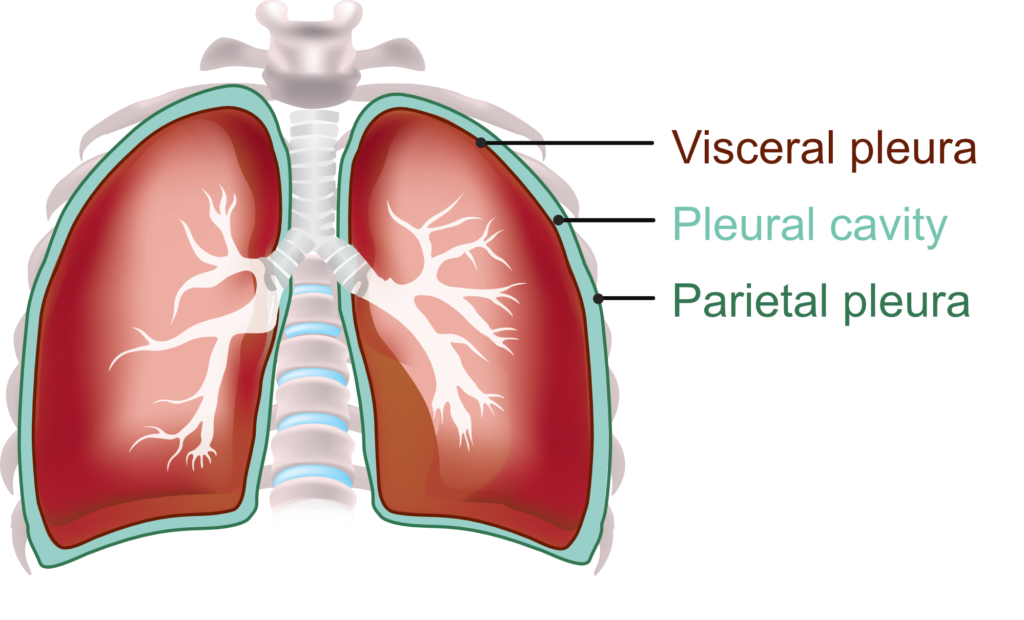 Our lungs don’t have muscular tissue, so we cannot move them at will. Instead, the lungs expand and shrink because of an intricate interplay between pressure and volume within the lungs themselves, the pleural cavity that separates the lungs from the rib cage, and the atmospheric pressure around you. The outer surface of the lungs (visceral pleura) clings to the inner surface of the ribcage (parietal pleura) with a pleural cavity in between. Your rib cage expands on the inhale and pulls on the lungs, which forces them to expand. This is called lung compliancy, the ability of your lungs to be stretched out following the movement of the rib cage. But your lungs also contain elastic fibers, which make them shrink back. When you reach the end of your inhalation, your lungs pull your thoracic cage inward as they recoil. This is called lung elasticity. The outward pull of the rib cage on inhale and inward pull of the lungs on exhale form your breath cycle. Proper lung function depends on the delicate balance between lung compliancy (ability to stretch out) and elasticity (tendency to recoil).
Our lungs don’t have muscular tissue, so we cannot move them at will. Instead, the lungs expand and shrink because of an intricate interplay between pressure and volume within the lungs themselves, the pleural cavity that separates the lungs from the rib cage, and the atmospheric pressure around you. The outer surface of the lungs (visceral pleura) clings to the inner surface of the ribcage (parietal pleura) with a pleural cavity in between. Your rib cage expands on the inhale and pulls on the lungs, which forces them to expand. This is called lung compliancy, the ability of your lungs to be stretched out following the movement of the rib cage. But your lungs also contain elastic fibers, which make them shrink back. When you reach the end of your inhalation, your lungs pull your thoracic cage inward as they recoil. This is called lung elasticity. The outward pull of the rib cage on inhale and inward pull of the lungs on exhale form your breath cycle. Proper lung function depends on the delicate balance between lung compliancy (ability to stretch out) and elasticity (tendency to recoil).
If your lungs lose their compliance (ability to stretch out), taking air in will become very difficult because your lungs want to shrivel. This happens if the tissue of the lungs becomes very fibrous, like in pulmonary fibrosis.
If your lungs lose their elasticity (ability to recoil), exhalation will become very difficult, since the lungs are no longer able to recoil naturally without effort. This happens with some respiratory diseases, like emphysema.
Your lung compliance is also directly linked to the mobility of your rib cage. It is the expansion of your rib cage that pulls on the lungs to make them expand on inhalation. If your rib cage cannot expand properly because of inflammatory arthritis or sedentary lifestyle in a collapsed posture, your lungs won’t be able to expand properly either and will gradually lose their compliance (ability to stretch out).
Unfortunately, the natural aging process is not kind to our lungs either. It affects your lung function in the following ways:
- As you get older, the elastic tissue throughout the body deteriorates, which means that your lungs will gradually lose their elasticity and, as a result, their vital capacity.
- Your rib cage stiffens with age because your intervertebral disks narrow and stiffen, which changes the articulation between ribs and vertebrae. It is usually accompanied by decreased elasticity of intercostal muscles. All those factors together compromise inspiration and decrease the elastic recoil of expiration. As a result, it becomes harder to take a breath because muscles of respiration must work harder during inhaling to counteract the stiffness.
- If you have slight forward head and slight kyphosis (rounding of the upper back) now, it tends to exaggerate with age. This can alter the position of both ribs and diaphragm, which leads to decreased efficiency of inspiration.
- All muscles in the body gradually lose strength and endurance with age. This applies to muscles of respiration as well (diaphragm, intercostals and others). This means that the muscles fatigue more easily, especially when they have to work harder (for example, during physical activity). The effect is amplified if there is an underlying lung condition.
As a result, it is expected that the lungs will lose 12% of capacity between the age of 30 and 50 and continue a steady decline from there. By age 80 we would usually lose about 30% of our lung capacity. It is not all doom and gloom, however. It doesn’t mean that as we get older, we are destined to go through steady decline in our lung function.
There are specific things we can do in our yoga practice to maintain healthy lung function. To keep proper balance of compliancy and elasticity of the lungs, we need to exercise both (although, depending on your health condition, one might be more important than the other). We support lung compliance by breathing in fully, expanding the ribcage and holding the air in. We support lung elasticity by exhaling fully and holding the air out.
In yoga, we work on maintaining and expanding lung compliancy and elasticity by:
- Increasing breath threshold – we can consistently work on deepening our inhalation and lengthening our exhalation both on our asana and pranayama practice,
- Working with breath retention – we can hold our breath in or out, which divides the breath into four different parts: inhale, hold after inhale, exhale, and hold after exhale. We can work with specific proportional relationships between those four parts and learn to hold our breath for longer periods of time. This is called the science of ratio. Read more about ratios >
- Dealing with the stiffness of the ribcage by doing all five directions of spinal movements (forward bends, back bends, side bends, twists, and axial extension postures). This helps maintain spinal mobility and elasticity of the intercostal muscles. Backbends, in particular, are effective for preventing “chest barreling” and an increase in kyphosis. To get the most out of those positions, we need to move into them and breathe deeply in those positions for some time (potentially adding breath ratios for better effect).
Since vital lung capacity is essential to health, it’s worth putting some effort into keeping our lungs healthy and resilient, which, hopefully, can slow down the respiratory decline associated with aging.

Your body consists of about 37 trillion cells; each of those cells knows exactly what to do to keep you alive and healthy. Together they perform an unquantifiable number of tasks in almost perfect harmony.
Resources
- Vital capacity as a predictor of cardiovascular disease: The Framingham Study (1983)by W.B. Kannel, M.D., Helen Hubert, Ph.D., and E.A. Lew, A.M., FSA.
- Lung Function May Predict Long Life or Early Death (2000) by Science Daily
- Why Does Lung Function Predict Mortality? Results From the Whitehall II Cohort Study (2010) by Severine Sabia, et al.
- Association of lung function with cardiovascular risk: a cohort study (2018) by Bin Wang, et al.
- Aging and Activity Tolerance \ Orthotics and Prosthetics in Rehabilitation by Ethan A. Hood, Kevin K. Chui, Michelle M. Lusardi
- Breath: The New Science of a Lost Art by James Nestor
- Respiratory| Compliance and Elasticity (video) by Ninja Nerd Lectures
- Respiratory| Mechanics of Breathing: Pressure Changes (video) by Ninja Nerd Lectures









Thank you Olga
Once more, really informative and stimulating read!
Much appreciate your work
Marielle
Thank you Mariellle!
Interesting, thanks Olga! Makes we want to get my vital capacity measured. Also wonder why, if there is such a strong independent association with cardiovascular morbidity, this isn’t a part of routine health screening over a certain age, like ECGs or stress tests?
I know, I was thinking the same – where can I get a spirometer? 🙂 I am not sure why they don’t do it in routine health screenings. I know that in long-term heart studies that I mention in the article the researchers started measuring FVC long before they realized its importance. So it is surprising that doctors don’t do it routinely. Seems like a pretty straightforward and non-invasive test.
A great article Olga! I really appreciate how skilfully your condense complex information into concise accessible reading.
The relationship between spinal and chest mobility and breathing is co-incidentally something I’ve been exploring in my practice recently as I’ve noticed that stabilising practices that used to be good for me when I was younger seem to be less so. My back and chest had begun to feel stiff and movement less fluid. Combining yogic breathing with some subtle Feldenkrais exercises has been very beneficial.
Great article once again!
What examples would you say, seated on the chair would be:
* Side Bends and
* Axial Extension Postures
I’m thinking seated lateral flexion, and maybe interlaced arms up over head?
Excellent! Thank you 🙂
Excellent!
Recently had surgery on my right carotid artery to remove a blockage. After surgery, I was tested frequently for FVC and handgrip strength. Now, after three weeks of recovery, I am back into walking hills, biking and paddling. Oh, and incorporating more twisting postures into my personal practice. I am now ready to begin Viniyoga therapy training in October. Great article, Olga!
Wonderful article
Awesome article! I cannot wait to share the insights gained with my students. Thank you!
You did again. Wonderful article. I think you should be taking more than 5 hours to digest, assimilate, put it again on the platform in the website. Great service. God bless!