Recent guidelines about dealing with back pain: do they make sense?
A recent article in the New York Times discussed the updated guidelines by the American College of Physicians regarding the treatment of lower back pain. While in the past, medication was recommended as the first remedy, “the new guidelines said that doctors should avoid prescribing opioid painkillers for relief of back pain and suggested that before patients try anti-inflammatories or muscle relaxants, they should try alternative therapies like exercise, acupuncture, massage therapy or yoga. Doctors should reassure their patients that they will get better no matter what treatment they try, the group said.”(1)
A big part of it, of course, is the recent epidemic of opioid addiction, which often starts with using opioids to manage back pain or other aches. Many doctors are concerned about that and are much more cautious now with prescribing muscle relaxants and other medications. The article quotes Dr. Weinstein, who said that patients have to stay active and wait it out. “Back pain has a natural course that does not require intervention,” he said. He added: “I know your back hurts, but go run, be active, instead of taking a pill.”(1)
Personally, I am a bit skeptical about Dr. Weinstein’s recommendation to “go for a run” or just return to normal daily activities following a back pain episode. Often, back pain sufferers cannot walk or have trouble getting out of bed, so running seems a bit premature. As for “returning to normal daily activities,” – often, those “activities” (or habitual movement patterns in our daily lives) led to the pain episode in the first place. Just returning to doing the same things we were doing before seems similar to the definition of insanity, which is “doing the same thing and expecting a different result.” Here, an investigation is in order to figure out if the way we hold and move our bodies in our daily lives is causing the problem or contributing to it.
As you might expect, the readers’ comments to the article were quite divided and generally fell into one of two camps: a camp that agrees that resuming normal activities and waiting it out is the best course of action and a camp of hurt, indignant readers who had suffered through debilitating back pain and/or discovered that their back pain indicated much more serious problems, like spinal abnormalities or bone cancer.
What do we do about back pain? Do we follow the new recommendations and just wait it out, or try to do everything we can to figure out where it is coming from and “fix it” somehow? We can find reasonable arguments for each approach. I do not pretend to have all the answers, but one thing seems pretty clear – your back pain might be entirely different from my back pain, so some sort of investigation seems appropriate to rule out more serious issues.
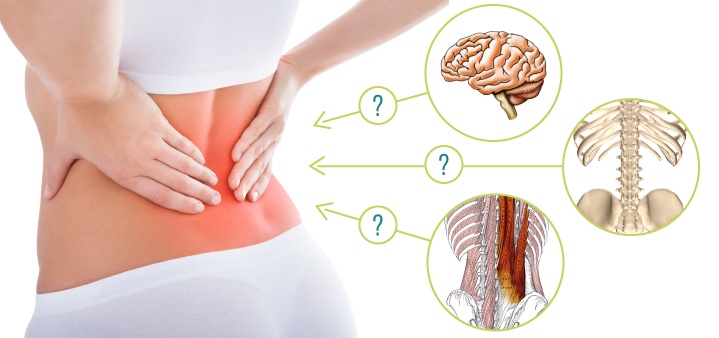
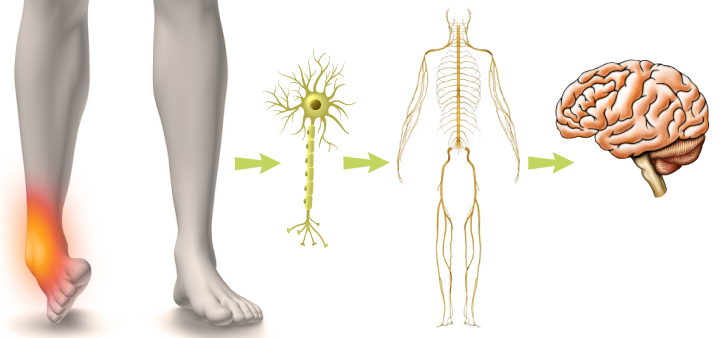
What kind of investigation is necessary? Here is the tricky part. According to the article, “scans, like an M.R.I., for diagnosis are worse than useless for back pain patients, members of the group said in telephone interviews. The results can be misleading, showing what look like abnormalities that actually are not related to the pain.” Even if a doctor sees a herniated disk on your scan, it may or may not be the cause of the back pain. This points to the trickiest issue with pain: recent science on chronic pain states that the experience of pain anywhere in the body has very little to do with the actual tissue injury. Let that sink in for a moment. The fact that your back hurts doesn’t mean that your back is injured. That seems entirely counterintuitive. “Pain is not just a message from injured tissues to be accepted at face value, but a complex experience that is thoroughly tuned by your brain.”(2)
Well, that certainly won’t show up on the lower back scan. After all, the chronic pain IS in our heads, only not in an offensive way that it is imaginary. No, the pain is real, but it is your brain’s interpretation of your experience that is influenced by many, many different factors. The longer the pain persists, the less it is connected to the state of the tissues (even if the initial pain was caused by something obvious, like a car accident). The article discussed above makes a reference to the brain’s involvement in the pain experience by quoting another doctor. Dr. Standaert says that for lower back pain sufferers to get better, “they have to believe their life can get better. They have to believe they can get to a better state.”(1)
Well, then, if the pain is regulated by your brain, can you think your pain away? It’s a bit more complicated than that. Multiple body systems are involved in the experience of pain, so healing also needs to happen on multiple levels. It’s a good thing that yoga has tools that affect the body on different levels, way beyond just basic stretching. It is wonderful that yoga is recognized in the article as one of the alternative therapies that can help with back pain, but we also know that there are all kinds of yoga out there; not all of them would be effective for pain management, and some could make things worse.

What kind of yoga would be helpful? Which yogic tools should we utilize to help ourselves and our students deal with chronic pain? Let’s explore.
Resources
Lower Back Ache? Be Active and Wait It Out, New Guidelines Say by Gina Kolata
Pain is weird by Paul Ingraham (Painscience.com)









Thank you! I am looking forward to this.
I saw that recent article too; I think it was good in theory, but a bit misguided. My guess is that they were trying to say that it is better to keep moving than the traditional recommendation of rest. But what you said totally makes sense–i.e., if one moves in the way that caused the pain in the first place, that may well just make things worse! 😮
Great timing! I’ve been reading a lot about the back. I’m currently reading Back Mechanic by Stuart McGill, PhD. I’m looking forward to your blogs!!!!
Looking forward to your 12 week class on pain.
Thank you ice again for a thoughtful post. I am looking forward to reading more!
Looking forward to this too. Having chronic lower back pain, and having a daily yoga practice, I have become frustrated that I am unable to do many forward bends and twists as they tend to make my back feel worse. I tend to spend most of the practice in variations of Bhujangasana as that always seems to improve things. Hoping your articles will help me be able expand my practice a little.?
Thanks for this new journey. Cannot wait to read more
Hi
What an interesting article , an applies to one an all . You either have had a back pain or you are going to get one . Looking forward to reading more .
John
Hhhmmmm,,,,, for years I ve been having quided back injections in Calgary…immediate pain relief but of course it’s an ongoing treatment…and I even tried a nerve block….nope…still pain. I ve been a hairdresser for many years,not in the best shape. until recently I just decided no more to the injections and I started doing easy floor excercices….faithfully and simple lunges and started noticing my thighs and waist line trimming . I m not gonna lie….i love yoga and it’s many benefits but there are certain poses I modify for my back just making sure to try and enjoy the practice rather then making it about myself ‘against’ yoga. i love Lakota arthritis gel for my back….it’s natural and really works. but that’s just my journey…
I would love to download your app but it’s only on the Apple App store. Can you make it available for Android phones as well. Thanks.
Hi Bev! We are planning to release the Android version of the app some time in April. Thank you for your interest!