Where to begin with spondylolisthesis and back pain


A new client contacts you about ongoing pain that bothers him most in the mornings and after athletics that include running. He reports, and your observations confirm, lower back pain plus hamstring tension that impact his ability to walk and move comfortably. Now in his early 40’s, he would like to feel better at work as well as at play with his young kids. He tells you that he has a medical diagnosis of spondylolisthesis. As a Yoga Therapist, where do you begin?
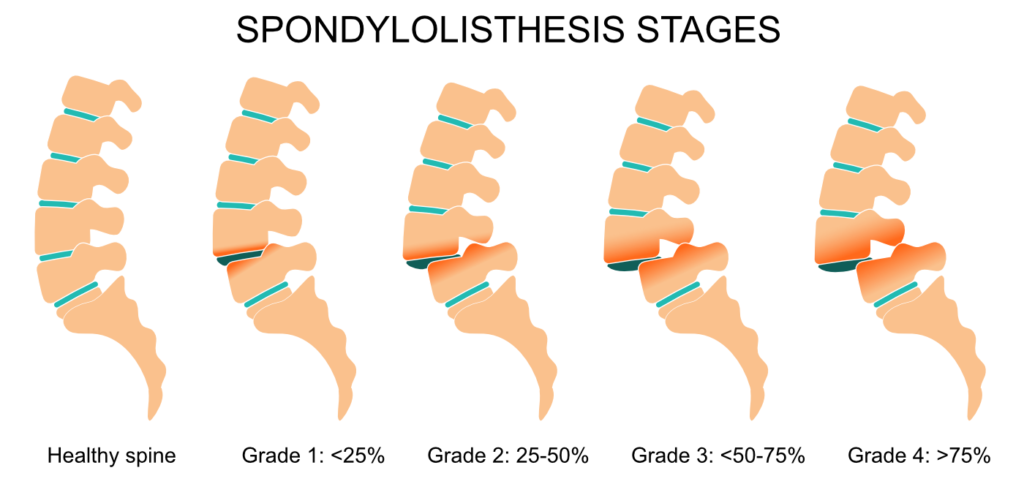
Spondylolisthesis is a condition of instability of the spine in which a vertebra of the spinal column has slipped forward and puts pressure on a nerve. (Not to be confused with spondylosis, fracture of a small spinal bone between two vertebrae, which may precede spondylolisthesis.) This can lead to back pain and/or leg pain. Surgery may be recommended, for some, depending upon the severity (or “grade”) of vertebral slipping and the resulting pain.
It would be favorable to work with someone with this condition individually, rather than in a group class setting. It is different from chronic, non-specific low back pain. Also, with the client’s permission, it is essential to consult with the practitioners or medical professionals who have diagnosed or treated them. Note this blog post is not medical advice nor a list of postures or sequencing to be generally applied; rather, it offers a few potential starting points for the Yoga Therapist to consider.
One general principle: avoid back extension. Back bends potentially could push the vertebra further forward and exacerbate nerve pain. Contraindicated yoga postures may include back bends like cobra (Bhujangasana), locust (Salabhasana) or upward-facing bow (UrdhvaDanurasana), and perhaps even the “cow” back extension in Cat-Cow. You may see that some of these postures are included in sequences that are recommended for other forms of chronic back pain. It’s essential to know as much as possible about your client’s situation before offering them a specific practice.
A research study to analyze injuries associated with yoga practice found spondylolisthesis in 16.9% of patient records. The investigators caution against “positions involving extreme spinal flexion and extension,” for spondylolisthesis and other conditions, as these kinds of injuries may be caused or exacerbated by yoga practice (Lee et al, 2019).
Research studies of yoga for low back pain also have excluded “persons whose back pain was attributed to a specific cause (e.g., spondylolisthesis),” (Sherman, 2005 & 2011). Thus, our yoga research doesn’t yet confirm what we may learn in yoga theory and observe anecdotally or experientially related to possible benefits of therapeutic yoga practices and Yoga Therapy.
Yoga Therapy can offer potential benefits not only structurally but for the whole person. These benefits include finding a comfortable resting position, and valuing rest; breathing practices repatterning the nervous system response; strengthening and stabilizing the core, and deep front line; developing postural awareness to lengthen and maintain axial extension. Yoga Therapy also offers reflections and contemplative practices as methods to build acceptance, self-awareness, and confidence.
Rest. If the client has difficulty relaxing or resting well due to pain and discomfort, allow ample time for them to explore how to find a comfortable resting position. This might be Constructive Rest (lying supine with knees bent and feet on the floor). A guided body scan or “compare and contrast” approach can help— for example, I learned from one of my mentors to compare the felt sense of a straight-legs version of Savasana (knees bent versus legs stretched out) with that of knees-bent in Constructive Rest. In a longer restorative posture, support the client’s joints in flexion and teach conditions and positions that invite the relaxation response.
Breathe. How you proceed with the breath depends on how the client shows up. A good place to begin is breath observation with the client learning, through direct experience and self-study, about their breath patterns and habits. This is an opportunity to educate them about benefits of nose breathing and how breathing affects every system of the body, as well as how we relate to discomfort, stability, and ease.
Stabilize. The word “spondylolisthesis” contains a reference to “slipping.” One of the body’s key structural elements, a spinal vertebra, has slipped out of place with painful consequences. Work with the client to develop awareness of alignment and other forms of stability. This likely involves gradually strengthening the abdominal muscles (the deep front line). It may also involve growing their confidence with a developmental approach to movement.
Lengthen. Offer postures that introduce attention to lengthening, or axial extension (not back-bending) along the vertical axis of the spine. In standing postures, lengthen from tail to crown in Standing Mountain (Tadasana), Reaching Mountain (Urdhva Hastasana), Awkward Pose (Utkatasana), and perhaps even Half-Dog at the Wall (Adho Mukha Svanasana standing variation). In supine postures, if there is hamstring tension, you may want to explore a modified, reclining Supta Padangusthasan I. At first, keep heels on the floor (lengthen legs horizontally rather than vertically); only later, add a vertical reach (legs lifting perpendicular, or at a lesser angle, to the floor).
Reflect. With guided meditation, reflection, and other forms of contemplation the client may shift how they relate and respond to limitations and discomfort. Offering them formal, guided loving-kindness and compassion meditations may be helpful. Or simply allow time in each session for them to report back about their practice at home, and then reflect back the understandings and insights they share.
Consider how you will respond if a client wants to do movements and activities that are questionable or contraindicated, such as a particular posture or form of exercise they really enjoy. Others may have told them these are OK to do. This can come up regardless of the limiting health condition; we all eventually negotiate this with ourselves, as well as with our students and clients. The art of Yoga Therapy sometimes is in finding a “middle way,” locating enjoyment and confidence alongside modifications or adaptations that support healing, or at least prevent further injury and pain. Future suffering is to be avoided (sutra 2.16).
For one person with spondylolisthesis, with whom I worked for several years, a combination of graduated, small movements and improving breath awareness was most helpful. Once we had progressed to standing postures, he walked away with experiences of grounding, stabilizing, and lengthening. He was able to support himself better from the inside out and brought this into all aspects of life. He gained confidence about what he could do, and how to gauge that and communicate from that place of awareness.
The final post in this blog series will delve into scoliosis as another relevant condition of the spine for some Yoga Therapy clients with back pain.
© 2022 Rachel Lanzerotti, Five Rivers Yoga LLC
Read more of Rachel’s posts on working with back pain >
Check out Rachel’s Real-Life Case Studies video series, available exclusively to Sequence Wiz members. Learn more about Case Studies at Sequence Wiz >)
Part 1: What questions to ask about lower back discomfort
Part 2: Using small movements and postural awareness to relieve pain and increase confidence
Part 3: Using chakra exploration and bija mantra to strengthen from the ground up
Part 4: Using restorative poses, asymmetrical movement, and directed breathing to heal physically and physiologically
+ Virtual event: A chat with Rachel on how to help your students take the load off their back
About Rachel
Rachel Lanzerotti (MSW, E-RYT500, IAYT-Certified Yoga Therapist) is the Founder of Five Rivers Yoga Therapyand creator of The RE/ST Method for Pain Recovery™. She is a Body-Mind Yoga Therapist, meditation teacher, counselor, health educator and specialist in back pain relief. Rachel has taught at UCSF Osher Center for Integrative Medicine and Spirit Rock Meditation Center.
She holds a BA in Human Biology from Stanford University and Master of Social Work (MSW) from San Francisco State University. For a decade prior to founding Five Rivers Yoga Therapy, Rachel ran an organizational consulting practice with community-based groups. She spent many years focused on direct action work for nonprofit and social change organizations.

Resources
Lee M, Huntoon EA, Sinaki M. Soft Tissue and Bony Injuries Attributed to the Practice of Yoga: A Biomechanical Analysis and Implications for Management. Mayo Clin Proc. 2019 Mar;94(3):424-431. doi: 10.1016/j.mayocp.2018.09.024. Epub 2019 Feb 18. PMID: 30792066.
Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, Deyo RA. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011 Dec 12;171(22):2019-26. doi: 10.1001/archinternmed.2011.524. Epub 2011 Oct 24. PMID: 22025101; PMCID: PMC3279296.
Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005 Dec 20;143(12):849-56. doi: 10.7326/0003-4819-143-12-200512200-00003. PMID: 16365466.









I really enjoyed this article, and hope many yoga teachers will read it too! If I had followed standard advice I could have hurt myself more. I am a RYT500 yoga teacher with grade 3 spondylolethesis. As a student, yoga saved me from having to have surgery, and I learned to adapt my practice to build core and back strength. My favorite pose has always been downward facing dog, with a chair or an assist to pull back the hips and extend the spine. Forward folds also bring great relief.
I doubted whether I could teach as I was going through my 300 hour training at Kripalu…. And then I realized I could help people who want to adapt their practice, especially as they get older. This obstacle became the way for me to support others in their yoga journey. Namaste
Hi Val!
Thank you for sharing about how you adapted your practice. I’m so happy to hear that you found this obstacle transformed into an offering. Namaste.
Thank you. As yoga teacher, and retired RN, dealing with low back and hip issues I very much relate to your article. I am fine tuning my personal practice and working with an amazing physical therapist. From a very active strong professional life and yoga practitioner I am interested, or forced
into a different approach. A gentler practice. Love to follow you and hear more.
Hi Paula!
I’m appreciating what you wrote about fine-tuning, with different approach and gentler personal practice. Thank you for your comment!